
PCOS (Polycystic Ovary Syndrome)
a most common hormonal disorder in women of reproductive age
PCOS is a hormonal condition, affecting up to one in 5 women of childbearing age, with up to 70% of affected women remaining undiagnosed.³
It is one of the manifestations of Metabolic Syndrome (MB), also called insulin resistance syndrome. Metabolic Syndrome is a cluster of various physical and metabolic abnormalities, including high blood glucose levels (hyperglycemia), high blood insulin levels (hyperinsulinemia), high blood pressure (hypertension), glucose intolerance and visceral obesity.9, 10
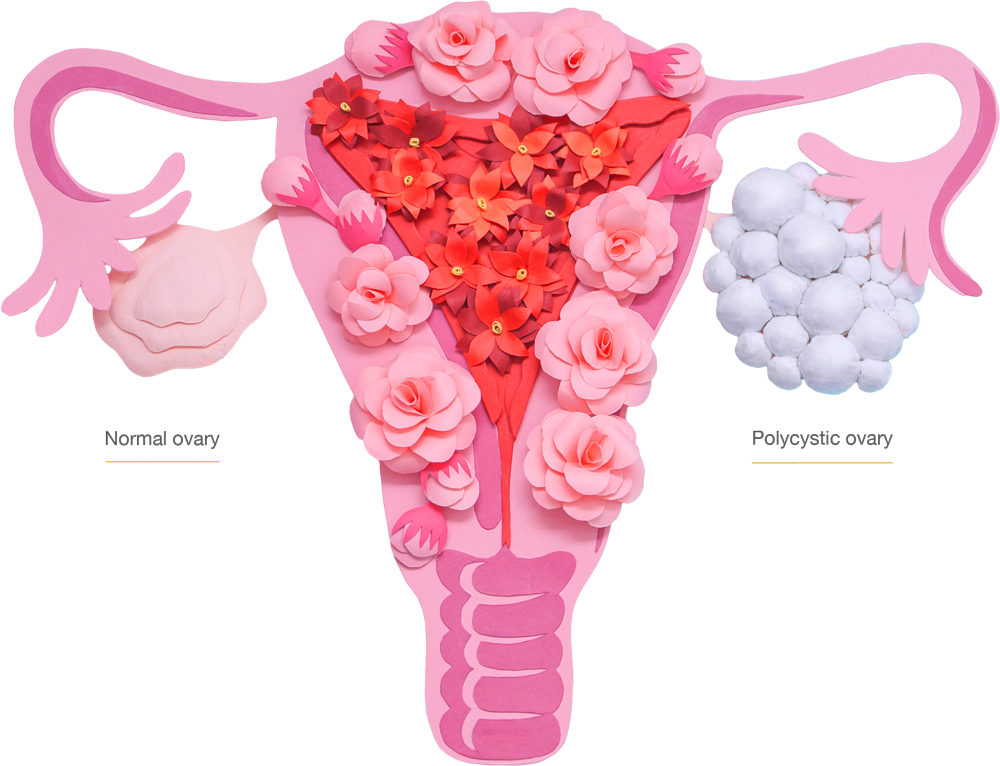
In a woman with PCOS, hormonal disbalance disrupts normal function of ovaries, the eggs often don’t fully develop and ovulate, therefore they cannot be fertilized.
PCOS symptoms
Signs and symptoms of PCOS vary. The most common PCOS symptoms include:
- Irregular, infrequent periods (irregular ovulation) or no periods at all (anovulation), prolonged menstrual cycles and abnormally heavy periods.
- Difficulty getting pregnant as a result of irregular ovulation or failure to ovulate.
- Excess androgen levels: high levels of testosterone (“male hormone“) in body, which may cause physical signs such as excess facial or body hair (hirsutism), thinning hair and hair loss from the head, oily skin, acne.
- Polycystic ovaries: ovaries become enlarged and contain many underdeveloped follicles which each contain an egg.
- Mood changes – including anxiety and depression. Obesity.
- Sleep apnea (sleep disorder when a person’s breathing is interrupted during sleep).
Not all women with PCOS will have the same signs and symptoms.
Symptoms can also change with age.
How is PCOS diagnosed?
If your doctors suspect that you have PCOS, they will evaluate a combination of clinical findings such as signs and symptoms, medical and family history and will perform a series of tests to confirm your diagnosis, including:
- Physical examination
- Blood tests
(for cholesterol, glucose, level of androgens, testosterone)
- Ultrasound
(to assess the ovaries’ appearance)
A diagnosis of PCOS is made when you experience at least two of these signs:
Irregular periods, excess androgen levels, polycystic ovaries visible via ultrasound

PCOS-related health conditions
Women with PCOS are at an increased risk of preterm birth, miscarriage, still birth, longer time to conception and poor embryo development. During IVF procedures woman with PCOS are a at an increased risk of reduced embryo implantation rates, ovarian hyper stimulation syndrome (OHSS) and ectopic pregnancy (pregnancy, when a fertilised egg implants itself outside of the womb) which are also exacerbated by obesity. 1, 3, 4, 5
Other conditions linked to the syndrome are high blood pressure and dyslipidemia (abnormal level of cholesterol and other lipids).
Insulin Resistance – a root cause of PCOS
It is thought that insulin resistance is a key factor in PCOS.
Insulin resistance is a decreased ability of the body to respond to the effect of insulin, a hormone that helps transport glucose into the body’s cells, where it is needed for energy production.
Normally, your digestive system breaks down carbohydrates into glucose, which then passes from your intestine into your bloodstream. As your blood glucose level rises, your pancreas secretes insulin into your bloodstream. Insulin allows glucose to move into your body cells from your blood. Once inside a cell, the glucose is used to produce energy.
Due to defect(s) in the insulin signal transduction pathways, cells do not respond to insulin and do not let glucose enter into the body cells. Glucose remains in the bloodstream. The body tries to compensate high circulating blood glucose levels (hyperglycemia) by making even more insulin and releasing it in the blood. Too much insulin (hyperinsulinemia) causes increased androgen (male hormone testosterone) and increased luteinizing hormone (LH, responsible for ovulation) production.
Higher levels of testosterone in women cause symptoms such as extra body hair, scalp hair loss and acne. Increased luteinizing hormone (LH) production causes deficiency of FSH (follicle stimulating hormone, responsible for the development and maturation of the ovarian follicle to the point of ovulation).
Disbalance of both follicle-stimulating hormone (FSH) and luteinizing hormone (LH) arrests follicular growth, maturation and damage oocyte quality. The eggs in underdeveloped follicles cannot mature and give rise to the cysts seen in patients via ultrasound.
The causes of impaired insulin signaling are complex and not well understood, but there is thought genetics, aging and ethnicity play roles in developing insulin insensitivity. Diet high in carbohydrates, being overweight or obese and physically inactive, stress and smoking adds to your risk.


Managing PCOS related fertility problems
PCOS cannot be cured, but good management can eliminate or improve the symptoms and reduce the long-term effects on your health.
Reduction of insulin resistance and hyperandrogenism (too high male hormons levels) together with ovulation promotion are key methods used to restore fertility in PCOS.
Insulin-sensitizing agents have been recently proposed as the therapy of choice for PCOS, since impaired insulin signaling (insulin resistance) with hyperglycemia and associated hyperinsulinemia are recognized to play a key role in development of the syndrome.11,12
The novel international evidence-based guideline for the assessment and management of PCOS recommends to assess the glycemic status (glucose level) in all women with PCOS. The same guideline marks that „blood glucose (…) should be optimized to improve reproductive and obstetric outcomes“.5
Insulin sensitizers help to increase insulin sensitivity, thereby regulating the amount of glucose (sugar) in your blood and decreasing blood insulin levels. This therapy has been associated with a reduction of serum androgen levels, with a decrease in hirsutism and acne, with a regulation of menses, with and an improvement of ovulation and fertility. 11,12
Healthy lifestyle, being physically active, losing 5-10% of your body weight are additional contributors to condition management.

WHY INOVO®
Inovo® is a scientifically substantiated formula to address the root cause of PCOS – insulin resistance – through:
- activation of two main insulin signaling pathways;
- decrease of too high levels of glucose, insulin and male hormons;
- Improvement of ovulation frequency and oocyte quality.
CHROMIUM PICOLINATE
Chromium is an essential trace mineral required by the human body for normal carbohydrate and lipid metabolism*. Nutritional chromium it is not made in the body and a certain level is needed in the diet to maintain health. Chromium picolinate appears to be the most bioavailable and efficacious (the most easily absorbed and utilized by the body) form of chromium supplementation.13, 15, 20
Chromium has effects which potentiate the action of insulin, a hormone that is critical for the normal regulation of carbohydrate, lipid and protein metabolism, to stimulate glucose transport into cells.13, 14
Chromium Picolinate has been extensively studied for its ability to enhance body composition and in over thirty-five human clinical trials has been shown to reduce appetite, enhance weight loss, caloric reduction, and carbohydrate and glucose metabolism. In a key clinical study, chromium picolinate supplementation not only led to weight loss, but also favourable body composition changes, as the weight lost was 98% fat mass and only 2% lean body mass.22, 40
Growing evidence suggests that chromium supplementation, in the form of chromium picolinate, may improve insulin sensitivity and glucose metabolism in patients with glucose intolerance.

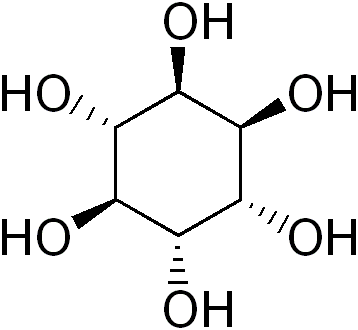
D-CHIRO-INOSITOL
D-chiro-inositol is a polyalcohol classified as an insulin sensitizer, one of 9 isomers of Vitamin B complex group. It is a naturally occurring substance produced in the human body from myo-inositol.
Inositol is an important component in all human cells. Inositol-containing lipids and phosphates are required for various structural and functional processes, including membrane formation, signaling (communication between cells and their surroundings) and osmoregulation (the process of maintaining salt and water balance (osmotic balance) across membranes within the body).23, 24
D-chiro-inositol also is important factor involved in insulin signaling, responsible for promoting glycogen synthesis and glucose utilization in cells.24, 25, 27
In patients with PCOS, D-chiro-inositol production from myo-inositol is impaired, deficiency of D-chiro-inositol is typical and considered to be early marker of impaired insulin signaling.25, 30
Clinical studies demonstrate d-chiro-inositol plays a role in supporting ovarian and menstrual function, healthy glucose and insulin metabolism, lipid metabolism, and cardiovascular function.26, 28, 30
D-BIOTIN
Biotin, also known as vitamin H, is a member of the B vitamin complex, necessary for both metabolism and growth in humans, particularly in the synthesis of glucose, production of fatty acids, antibodies, digestive enzymes and in tissue metabolism.30, 31, 32
Biotin helps to keep your skin, hair, eyes, liver, and nervous system healthy and is crucial nutrient during pregnancy, as it’s important for embryonic growth. Biotin contributes to the maintenance of normal mucous membranes, normal energy-yielding and macronutrient metabolism, helps to maintain normal psychological function.32
Recent scientific studies show biotin improves glucose tolerance and decreases insulin resistance and triglycerides in individuals with type 2 diabetes.33, 34, 35
Growing evidence suggests that addition of biotin appears to increase the insulin sensitizing effects of chromium.
Supplementation with a combination of chromium picolinate and biotin improves glucose management including enhanced glucose uptake and increased glycogen synthesis, decreases cholesterol levels and the risk of heart disease associated with diabetes.36, 37, 38, 39


CONSIDER INOVO® IF YOU SEEK FOR:
- correction of metabolic disorders (high blood glucose and insulin levels);
- decrease of hirsutism and acne caused by androgen excess;
- simple and safe method capable of restoring normal menstrual cycle;
- getting pregnant in a natural or medically assisted way;
- increased chances for successful IVF (in-vitro fertilization) procedures;
- reduction of appetite and enhancement of body’s fat mass loss;
- increase in energy level, stabilization of moods.
Useful references:
1. José Bellver, Luis Rodríguez-Tabernero, Ana Robles, Elkin Muñoz, Francisca Martínez, José Landeras, Juan García-Velasco, Juan Fontes, Mónica Álvarez, Claudio Álvarez, Belén Acevedo. Polycystic ovary syndrome throughout a woman’s life. J Assist Reprod Genet (2018) 35:25–39.
2. Uche Anadu Ndefo, Angie Eaton, Monica Robinson Green. Polycystic Ovary Syndrome A Review of Treatment Options With a Focus on Pharmacological Approaches. Vol. 38 No. 6 • June 2013 • P&T.
3. Carrie C. Dennett1 and Judy Simon The Role of Polycystic Ovary Syndrome in Reproductive and Metabolic Health: Overview and Approaches for Treatment. SPECTRUM.DIABETESJOURNALS.ORG.
DOI: 10.2337/diaspect.28.2.116
4. Per O. Dale, Tom Tanbo, Egil Haug, Thomas Åbyholm. The impact of insulin resistance on the outcome of ovulation induction with low-dose FSH in women with PCOS. Human Reproduction vol.13 no.3 pp.567–570, 1998.
5. PCOS International evidence-based guideline 2018.
6. Samir Bhattacharya et al. Mechanism of Lipid Induced Insulin Resistance: An Overview. https://www.researchgate.net/publication/276335137.
7. Samuel T Olatunbosun. Insulin Resistance. https://emedicine.medscape.com/article/122501-overview.
8. Max C. Petersen, Gerald I. Shulman. Mechanisms of Insulin Action and Insulin Resistance. 01 AUG 2018https://doi.org/10.1152/physrev.00063.2.
9. A.O. Oladejo. Overview of the metabolic syndrome; an emerging pandemic of public health significance. Ann Ib Postgrad Med. 2011 Dec; 9(2): 78–82.
10. Matthew B. Lanktree, Robert A. Hegele. Metabolic Syndrome. Genomic and Precision Medicine (Third Edition), 2018.
11. Renato Pasquali, Alessandra Gambineri. Insulin-sensitizing agents in polycystic ovary syndrome. European Journal of Endocrinology (2006) 154 763–775.
12. Marcos Felipe Silva de Sá. Widding the Use of Insulin Sensitizers to Patients with Polycystic Ovarian Syndrome-A Late, but Wise Decision Rev. Bras. Ginecol. Obstet. vol.41 no.3 Rio de Janeiro Mar. 2019 Epub May 16, 201.
13. William T. Cefalu, Frank B. Hu. Role of Chromium in Human Health and in Diabetes. Diabetes care, Volume 27, Number 11, November 2004.
14. Peter J. Havel. A Scientific review: The Role of Chromium in Insulin Resistance.
15. Scientific Opinion on the substantiation of health claims related to chromium. EFSA Journal 2010;8(10):1732.
16. Sedigheh Amooee, Mohammad Ebrahim Parsanezhad, Maryam Ravanbod Shirazi, Saeed Alborzi, Alamtaj Samsami. Metformin versus chromium picolinate in clomiphene citrate-resistant patients with PCOS: A double-blind randomized clinical trial. Iran J Reprod Med Vol. 11. No. 8. pp: 611-618, August 2013.
17. Sherif Ashoush, Amgad Abou-Gamrah, Hassan Bayoumy, Noura Othman. Chromium picolinate reduces insulin resistance in polycystic ovary syndrome: Randomized controlled trial. J. Obstet. Gynaecol. Res. Vol. 42, No. 3: 279–285, March 2016.
18. Siavash Fazelian, Mohmad H. Rouhani, Sahar S. Bank, Reza Amani. Chromium supplementation and PCOS: A systematic review and meta-analysis. Journal of Trace Elements in Medicine and Biology, 42, April 2017.
19. C. Leigh Broadhurst, Philip Domenico. Clinical Studies on Chromium Picolinate Supplementation in Diabetes Mellitus – A Review.
20. Opinion on the Tolerable Upper Intake Level of Trivalent Chromium. European Commission, Health & Conusmer Protection Directorate-General, Scientific Committee on Food, SCF/CS/NUT/UPPLEV/67 Final, 23 April 2003.
21. Anderson RA. Chromium in the prevention and control of diabetes. Diabetes Metab. 2000;26:22-27.
22. Kaats, G.R.; Blum et al. A randomized, double-masked, placebo-controlled study of the effects of chromium picolinate supplementation on body composition: A replication and extension of a previous study. Curr. Ther. Res. 1998, 59, 379–388.].
23. Arturo Bevilacqua, Mariano Bizzarri. Inositols in Insulin Signaling and Glucose Metabolism. International Journal of Endocrinology, Volume 2018, Article ID 1968450.
24. Simona Dinicola, Mirko Minini, Vittorio Unfer, Roberto Verna, Alessandra Cucina, Mariano Bizzarri. Nutritional and Acquired Deficiencies in Inositol Bioavailability. Correlations with Metabolic Disorders. International Journal of Molecular Sciences, 2017.
25. Jean-Patrice Baillargeon, Evanthia Diamanti-Kandarakis, Richard E. Ostlund, Jr., Teimuraz Apridonidze, Maria J. Iuorno, John E. Nestler. Altered D-Chiro-Inositol Urinary Clearance in Women With Polycystic Ovary Syndrome. Diabetes Care 29:300–305, 2006.
26. Cristiana Paul, Antonio Simone Lagana, Paolo Maniglio, Onofrio Triolo, David M. Brady. Inositol’s and other nutraceuticals’ synergistic actions counteract insulin resistance in PCOS and metabolic syndrome: state-of-the-art and future perspectives. Gynecol Endocrinol, 2016.
27. Maurizi AR, et al. A pilot study of D-chiro-inositol plus folic acid in overweight patients with type 1 diabetes. Acta Diabetol. 2017 Apr;54(4):361-365.
28. Sortino MA, et al. Polycystic Ovary Syndrome: Insights into the Therapeutic Approach with Inositols. Front Pharmacol. 2017 Jun 8;8:341.
29. P. Piomboni, R. Focarelli, A. Capaldo, A. Stendardi, V. Cappelli, A. Cianci, A. La Marca, A. Luddi, V. De Leo. Protein modification as oxidative stress marker in follicular fluid from women with polycystic ovary syndrome: the effect of inositol and metformin. J Assist Reprod Genet (2014) 31:1269–1276.
30. John E. Nestler, Daniela J. Jakubowicz, Paula Reamer, Ronald D. Gunn, Geoffrey Allan. Ovulatory and metabolic effects of d-chiro-inositol in the polycystic ovary syndrome. The New England Journal of Medicine, 1999.
31. R. Keith Campbell. A Critical Review of Chromium Picolinate and Biotin. US Pharm. 2006; 31(11) (Diabetes suppl)1-4.
32. Scientific Opinion on the substantiation of health claims related to biotin. EFSA Journal 2009; 7(9):1209.
33. Cristina Fernandez-Mejia, Maria-Luisa Lazo-de-la-Vega-Monroy. Biological Effects of Pharmacological Concentrations of Biotin. Journal of Evidence-Based Complementary & Alternative Medicine 16(1) 40-48 ª, 2011.
34. Dakshinamurti K, Tarrago-Litvak L, Hong HC. Biotin and glucose metabolism. Can J Biochem. 1970;48:493-500.
35. Furukawa Y. Enhancement of glucose-induced insulin secretion and modification of glucose metabolism by biotin. Nippon Rinsho. 1999;57:2261-2269.
36. Wang ZQ, Zhang XH, Cefalu WT. Chromium picolinate and biotin enhance glycogen synthesis and glycogen synthase gene expression in human skeletal muscle culture [abstract]. Diab Res Clin Pract. 2000;50:395.
37. Juturu V, Ruelle A, et al. Improved glycemic control after diabetes education and chromium picolinate/biotin supplementation in type 2 diabetes: Results from patients experience pilot program. Trace Elements Electrolytes. 2006;2:66-72.
38. Albarracin C, Fuqua B, et al. Effect of chromium picolinate and biotin combination on coronary risk lipids and lipoproteins in subjects with non HDL–C (>130 mg/dL) in type 2 diabetes mellitus [abstract]. Arterioscler Thromb Vasc Biol. 2005;25:E98-99 (abstr. P266).
39. Juturu V, Geohas J, et al. Chromium picolinate and biotin combination reduces coronary risk factors [abstract]. Arterioscler Thromb Vasc Biol. 2004;24:E66 (abstr. P88).
40. Darryn Willoughby et al. Body Composition Changes in Weight Loss: Strategies and Supplementation for Maintaining Lean Body Mass, a Brief Review. Nutrients 2018, 10(12), 1876; https://doi.org/10.3390/nu10121876.
